Claims Accession Value Assignment
Prior to Fusion v6.0, AML assigned the FIN Accession number based on one of the ORDX values received for the patient on a daily basis. That assignment created several issues because:
- Fast created a demographic file that was sent to FIN on a daily basis.
- Fast tried to anticipate what AML would use as the ORDX, or FIN Accession. The logic that AML used did not always match what Fast anticipated. This was further impacted when flexible routing was implemented in Fast.
- AML Accession, which corresponds with the ORDX value, was sometimes delayed or sent in a different billing file with a different ORDX.
These issues meant that patient demographics could be assigned to the wrong FIN Accession, and impacted sending accession level flags, for example the ABN flags.
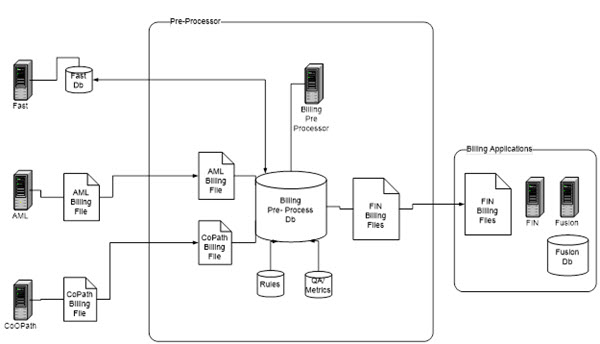
Fusion v6.0 Billing Data Concentrator
The Billing Data Concentrator (BDC) supports claims accession value assignments based on the following:
- Assignment of accession numbers for accessions from AML and CoPath.
- Matching demographics to the correct order.
- Ability to combine AML and CoPath billing onto one claims accession as necessary.
- Processing billing files for other systems that may require translations of billing codes and the default of some values such as client and bill to.
Assembly of Accession value logic includes:
- Patient ID (Foreign MRN) PID;2
- Lab code/MPI qualifier PV1;3 lookup client table to get MPI qualifier
- Lab system accession PID;3.1/ORDX
- Lab system account number PID;18
- Client code PV1;3
- Provider code PV1;8
- DOS (collect date) FT1;4
- Charge to or bill to comes from DFT messages
- Test lab department
- Test Code/billing code/cdm
- Separators based on age, and transmittal to FIN system
General Flow
- Inbound Concentrator creates an accession and then:
- Sets a database date flag field to note new data appears in the accession.
- Stores DFT demographics on the accession table.
- Stores BAR demographics in a separate table.
- Keeps the accession open a period of time depending on the:
- Presence of a final flag or receipt flag for the test.
- Need to have flag set for when ready to bill.
- Ability to always mark some tests as final.
- Cancellation = final.
- Sends the accession, or claim, to the billing system.
- Supports eMPI matching capability.
- Connects the accession to BAR demographics and eMPI right before it qualifies for scrubbing.
- If the accession has different BAR demographics then adds it to the accession table linking them by LIS accession.
- Next performs an eMPI match.
- Records eMPI enterprise FOID for the accession.
- Decides if need to use central patient detailed info on the accession.
- Is based on Lab code configuration.
- Is based on age of information on central patient.
- Scrub accession.
- Does not release to billing system until hold time is met.
- Sends accession to billing system.
- Sends HL7 to billing system to communicate patient and charge.
|
| This document contains confidential and proprietary information owned by the Rhodes Group, Inc. This Information may not be downloaded, copied, or transferred, in any medium, either in whole or in part, except as allowed by the Rhodes Group. Copyright 2017, Rhodes Group Inc. | |
| Version 6.0, Release 1
Reference Manual |
Prepared by Rhodes Group
September 2017 |
